Artificial intelligence (AI) has vast potential in the medical field. It’s particularly valuable in procedures like endoscopy that, despite being common, require complex analysis and expert insight. The health care industry hasn’t overlooked this opportunity, either, as early uses of AI in endoscopy have already driven promising results.
Endoscopy is the process of examining patients’ bodies using a thin, flexible tube equipped with a camera and light. While the procedure itself is fairly straightforward, making sense of the images can be challenging. AI has already offered solutions along several fronts.
1. Improved Abnormality Detection
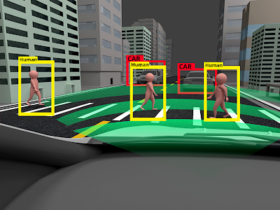
The most significant AI breakthrough in endoscopy is how machine learning improves detection. Endoscopes often search for small abnormalities like precancerous polyps or lesions. Early studies suggest machine learning can detect these warning signs more accurately than humans.
As early as 2017, AI algorithms could detect polyps with 86% accuracy, while expert doctors only achieved 74% accuracy. Since then, machine learning models have reached accuracies as high as 96.4%. Such systems can often spot abnormalities that humans may miss, too.
In practice, AI models won’t replace specialists. However, physicians can use them to gain greater confidence in their diagnoses without a time-consuming process. As a result, health care systems can give patients the help they need earlier in their conditions’ timeline, leading to improved outcomes.
2. More Reliable Classification
Accuracy isn’t the only benefit of AI in endoscopy. Machine vision models are also adept at classification — or differentiating between different types of detected abnormalities.
Classification is important because different types of polyps or lesions require different approaches to treat effectively. Consequently, AI models could ensure people get the care they actually need by detecting subtle differences between abnormal growths.
One neural network was able to distinguish between colorectal polyps with up to 87% accuracy, putting it on par with expert pathologists. Using this model, doctors could diagnose a patient without additional review, leading to quicker, more accurate treatment. In cases where the AI and initial diagnoses differ, the extra opinion could help staff consider additional possibilities to improve diagnostic confidence.
3. Streamlined Procedures
It’s also worth noting that endoscopy AI is fast on top of being accurate and specific. While certainty is the most important thing in a medical diagnosis, speed matters, too. A quicker process means treatment can begin sooner and doctors can see more patients in less time.
Some neural networks have proved effective at detecting polyps in real time, removing the need for post-endoscopy analysis for greater confidence. Other algorithms may not deliver immediate results but can take minutes instead of the hours or days a lab procedure would take.
When doctors can improve their detection and classification without taking additional time, it leads to dramatically improved patient outcomes. Earlier treatment aside, the time savings let a constrained workforce serve a larger number of patients, making turnover and labor shortages less impactful.
4. Lower Cross-Contamination Risks
The uses of AI in endoscopy go beyond the procedure itself. Preventing cross-contamination between tests is also important, as roughly one in 1,000 colonoscopy patients get infected from the process. AI can help by ensuring cleaner, safer storage and sanitization.
Smart drying cabinets employ HEPA filtration, positive pressurization, and similar steps to dry and disinfect endoscopes between procedures. Algorithms push them further by monitoring interior conditions in real time. They can then adjust settings as necessary to maintain sterile storage as cabinets open and close.
Alternatively, AI can predict equipment failures and alert staff of the issue before it compromises endoscope cleanliness. Processes like this are already common in smart homes and industrial HVAC equipment, but in the medical field, they could prevent infections and improve overall health.
5. Expanded Specialist Training
AI is also a useful training tool. Endoscopy is a complex, specialized process, but equipping prospective specialists with the necessary skills and knowledge is often too slow to keep pace with rising demand. Considering how the U.S. alone will be short 86,000 physicians by 2036, something needs to change.
Because AI is so accurate, it’s a helpful way to show trainees what various polyps, lesions or other abnormalities look like. Doctors in areas without as many expert specialists or other training equipment benefit the most from this use case. By using AI as a guide, they can quickly improve their detection and classification skills.
As AI streamlines specialist training, reliable endoscopy and related care will become accessible to more people. Such a shift could work against long-standing barriers to care between different demographics.
Potential Downsides to AI in Endoscopy
As beneficial as AI can be in endoscopy, it comes with a few drawbacks. Skewed training data can cause AI to amplify human biases, and many historical medical records lack equal representation. Consequently, these tools may not be reliable for every patient demographic.
Collecting enough data to train these models may also introduce privacy concerns. The health care industry faces strict regulations on patient data security, so it could be difficult to balance model reliability with cybersecurity and compliance.
Over-reliance on AI introduces another concern — such diagnostic tools are highly accurate but imperfect. Doctors may become complacent over time and take their input at face value, leading to rushed screenings and potential misdiagnoses. Such use cases would counteract the benefits of using the technology.
Using AI in Endoscopy Safely
Thankfully, there is a safe way forward. Once medical organizations recognize these downsides, they can build safer AI policies to mitigate the negative effects while capitalizing on the benefits.
Greater care during training is paramount. A diverse team must oversee development and frequently audit the algorithm to find and correct biased tendencies. During this phase, teams can also use synthetic data to protect patient privacy while providing a larger training database. Models trained on synthetic data can be more accurate than others, so it may be the best way forward, even outside of privacy and bias concerns.
Finally, health care systems must train doctors to use AI carefully. They must emphasize how human experts should always have the final say and teach professionals about AI’s shortcomings to prevent them from over-relying on the technology.
AI Is Driving the Endoscopy Field Forward
While challenges remain, it’s hard to overlook the potential of AI in endoscopy. Some hospital networks are already regularly using AI-assisted screenings, and as technology improves, its adoption will likely expand. Broader usage, in turn, will lead to growth in relevant datasets and the development of additional best practices.
As such trends continue, AI could reshape the field of endoscopy. These procedures will become more accurate, precise, accessible, efficient and safe. Both doctors and patients will benefit from that shift.