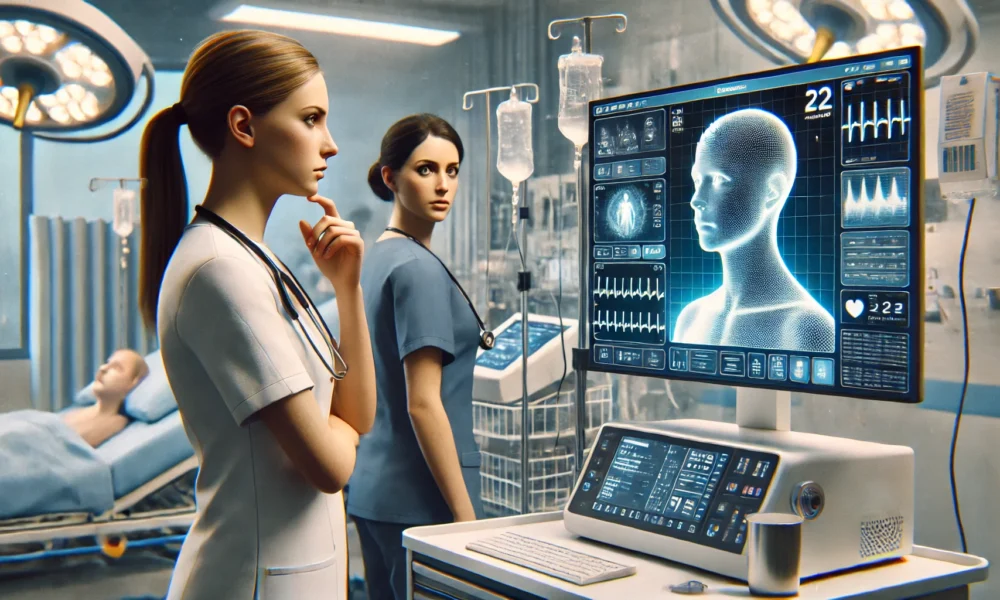
As a result of widespread burnout and labor shortages, the ever-changing healthcare space is always searching for the ‘next big thing’ to support workforce enablement, and AI is currently the leading contender. AI adoption is becoming increasingly prevalent in clinical settings and is here to stay, with industry executives reporting it is the most exciting and most improved technology for a fourth consecutive year.
However, while there are undeniably promising benefits, AI platforms specifically designed to improve the clinician experience have spurred skepticism, and many clinicians are still wary of its use – including nurses. In April 2024, San Francisco-based nurses employed by Kaiser Permanente protested the health system’s use of “untested” AI tools , with one major issue being the disrespect of the nursing profession at the hands of AI-enabled workforce enablement solutions. To mitigate this growing challenge, nurse leaders at Kaiser requested that workers and unions be a part of the AI development process, and that they independently determine how AI is used on an individual basis.
Within the profession, there is still underlying mistrust and hesitation with unfamiliar technology, as the safety and well-being of the patient is always the main concern. Nurses deserve the time, space, and resources they need to develop a genuine comfort level with AI by understanding the potential benefits to not only the patient, but to themselves, as when used successfully, AI solutions can supplement the nursing profession – not replace it.
Unparalleled Value of the Nurse Role
Across the industry, the fear that AI will be used in place of nurses is the most prominent cause of apprehension. The thought is that automated solutions may lead to shifts in staffing numbers and job roles, a particularly pressing concern amidst pervasive workforce deficits, which could lead to resistance from nurses who are worried about job security.
The nurses at Kaiser had repeated difficulties with an electronic health record (EHR) system’s AI-enabled tool that details patient care during each shift, and then harnesses the new data to dictate the degree of care a patient will need from nurses working the following shift. Historically, nurses had more control over establishing patient treatments. Now, nurses report that the new system routinely delivers insufficient staffing assignments to provide patient care because the system does not have the capacity to factor in important responsibilities such as preparing certain treatments before an appointment or educating patients and family members about their care plans. These seemingly trivial tasks can result in disastrous consequences including delayed or fragmented care, increased readmissions, or challenges related to medication adherence.
Another similar consideration is the dependability of human interaction during the treatment process. The human touch is one of the most pivotal aspects of patient care, at the core of nursing. Although AI can assist with accelerating data analysis and minimizing administrative burden, these solutions are unable to recreate empathetic, compassionate nurse communication. Delivering care with emotional support and understanding is irreplaceable, especially as trust and rapport between nurses and patients notably improves care outcomes.
Evaluating Accuracy and Privacy Concerns
Healthcare delivery demands unwavering precision and accuracy. As such, the notion that AI could negatively impact outcomes by misdiagnosing a patient or making incorrect treatment can be quite unnerving. Unlike mistakes made by humans which are typically predictable and easy to correct, AI-generated errors are more randomized, making them difficult to anticipate and rectify quickly, potentially leading to patient harm. This margin of error is too risky in healthcare, further contributing to uncertainty.
Healthcare AI usage has also prompted concerns tied to ethics and privacy. With healthcare data breach prevalence rising rapidly, patient data must remain confidential, and any incorporation of AI must include stringent measures to guarantee maximum data protection. Nurses feel personally responsible for maintaining patient confidentiality, and any lapses due to technological vulnerabilities are completely unacceptable.
Recognizing AI’s Undeniable Benefits
AI’s real opportunity is allowing clinical professionals to return to performing the tasks they were trained to do – and those that they genuinely love doing. AI can tackle the mundane, routine duties that hold clinicians back, providing them with increased bandwidth centered around direct patient care. This notion is fundamental to their reasoning of why they pursued their professions to begin with.
Comprehensive, personalized education is needed for nurses to fully absorb AI’s utility and accept AI as a viable professional asset. Take virtual reality (VR), for example – originally created to enhance the video game experience, the technology has expanded into many additional focus areas. Once the value of VR grew to be more prominent, curious minds across a wide array of occupations gradually began experimenting to determine supplementary applications. The same sentiment should be applied to AI’s initiation into healthcare in an effort to improve clinical outcomes by implementing technologies to focus on human-centered care delivery.
In healthcare, VR training produces engaging and immersive 3D perspectives of simulated, feasible scenarios using a digital headset that gives clinicians the opportunity to observe, listen, and feel their environment. Rather than delivering knowledge through instructor lessons, VR can optimize clinician preparedness by merging strategic components from online learning, video and multimedia-based learning, and simulation-based learning, enabling clinical professionals to learn from their mistakes without the risk of patient harm. VR training has been proven to enhance learners’ surgical performance by 230%, equipping them with the necessary skills to complete procedures 20% quicker and more accurately than traditional training modalities.
A Way Forward
Given these reasonable hesitations, AI-enabled practices in healthcare and nursing must take a cautious, meticulous approach with respect to the nurses in their organization. Primarily, nurses must be sufficiently educated that AI should serve as a tool to assist, not replace, the critical judgement and benevolent care nurses provide. Additionally, since most AI developers do not have clinical expertise, healthcare organizations should collaborate with nurses to increase user accessibility and make a lasting, positive impact on nurse sentiment towards AI.
Despite the advantages of leveraging AI-driven models in healthcare, nurses should not feel forced to adopt these technologies. Nevertheless, if hospitals are interested in introducing AI into clinical workflows, leaders should provide extensive training to facilitate seamless integration and thoroughly listen to nurses’ concerns to ensure they feel adequately heard. Balancing technological advancements with the incomparable human elements of nursing will optimize clinical outcomes and help build trust.