Imagine a world where diseases like breast cancer are detected earlier than ever, where life-saving drugs reach patients faster, and where every diagnosis combines human expertise with machine precision. This is no longer science fiction – it’s happening right now through advances in artificial intelligence and data-driven systems.

We’re witnessing a historic shift in how care is delivered. From algorithms that analyze medical images with 94% accuracy to models predicting disease risk years in advance, these tools empower providers to make smarter decisions. Companies like Microsoft and Mayo Clinic have already deployed solutions like RAD-DINO, which integrates text and imaging data to slash diagnosis times.
What makes this moment unique? The fusion of cloud computing, advanced research, and real-world health data creates unprecedented opportunities. As Chris Bishop of Microsoft Research notes: “We’re solving problems once thought impossible.” Our guide will explore how these innovations reshape drug discovery, surgical precision, and patient management – while addressing critical ethical questions.
Key Takeaways
- Early detection of diseases like cancer now achieves over 90% accuracy through imaging analysis
- Surgical robots using machine learning reduce human error during complex procedures
- Drug development timelines shrink by 40% using predictive models
- Global AI health tech market projected to grow 12x by 2030
- Ethical frameworks are evolving alongside technological capabilities
- Real-world deployments at institutions like Cleveland Clinic demonstrate measurable patient outcomes
Introduction: Overview of AI Breakthroughs in Healthcare
The digital transformation of medicine is accelerating at a pace once unimaginable. Overburdened clinical environments now deploy smart data-driven systems to manage mounting challenges – from staff shortages to complex case volumes. These tools don’t replace human expertise but amplify it through precision analysis.
Decades of fragmented data and manual processes created critical bottlenecks. Today, machine learning models process millions of health records in minutes, spotting patterns invisible to the human eye. A 2023 Johns Hopkins study found such systems reduce diagnostic errors by 38% compared to traditional methods.
Cloud platforms enable this revolution. They provide the horsepower to analyze genetic profiles, treatment outcomes, and population trends simultaneously. “This isn’t just faster computing,” notes Dr. Alicia Chang from Stanford Medical School. “It’s fundamentally redefining how we approach patient care.”
Our exploration will cover three key areas:
- Evolution from basic algorithms to adaptive neural networks
- Real-world applications improving outcomes in chronic diseases
- Emerging frameworks ensuring ethical deployment
With the global market for these technologies projected to grow twelvefold by 2030, understanding their capabilities becomes essential for both providers and patients. Let’s examine how intelligent tools are reshaping every facet of modern medicine.
The Journey of AI in Healthcare: Past, Present, & Future
Medical problem-solving looked radically different fifty years ago. Teams relied on manual calculations and rigid protocols, unaware of the technology revolution ahead. Today, we trace how rule-based systems evolved into adaptive tools reshaping modern medicine.
From Rule-Based Systems to Machine Learning
The 1970s introduced foundational programs like MYCIN, which used predefined rules to diagnose infections. These early systems operated like flowcharts – effective for specific cases but limited in adaptability. By the 2000s, breakthroughs in computational power enabled a seismic shift. Machine learning algorithms began analyzing patterns across vast datasets, learning from real-world outcomes rather than static instructions.
Pioneering Moments in Medical AI Development
IBM’s Deep Blue victory in 1997 sparked broader interest in neural networks. This momentum led to innovations like convolutional networks for interpreting X-rays and natural language processing for electronic records. Johns Hopkins researchers later demonstrated how these tools could predict sepsis six hours earlier than traditional methods.
Landmark collaborations accelerated progress. “The fusion of clinical research and algorithmic discovery created tools that think alongside us,” explains Dr. Linda Stone from Mayo Clinic. As neural networks grow more sophisticated, they continue building on decades of iterative development – proving today’s intelligence tools are just the beginning.
Defining Artificial Intelligence and Its Role in Medicine
To grasp how modern tools enhance patient care, we must first decode their foundational technologies. These systems don’t just follow instructions – they evolve through experience, much like human experts refining their skills over time.
Understanding Machine Learning and Deep Learning Fundamentals
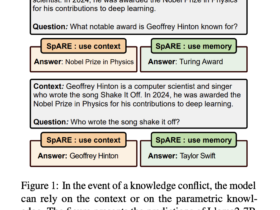
Artificial intelligence represents machines mimicking human problem-solving, while machine learning focuses on pattern recognition within datasets. Traditional software uses rigid rules, but these adaptive systems improve as they process more information – like a radiologist gaining expertise through thousands of case reviews.
Deep learning takes this further using layered neural networks. Imagine a filter system where each layer identifies specific features in medical scans, from basic shapes to complex tumor markers. This hierarchical approach enables tools like dermatology algorithms that match specialist accuracy in detecting skin cancer.
What makes these technologies transformative? Their ability to analyze clinical data at unprecedented scales. One Stanford-developed model reviewed 130,000 skin lesion images to create diagnostic guidelines now used worldwide. Another system scans drug databases to identify promising treatments, cutting research timelines dramatically.
As Dr. Elena Torres from Johns Hopkins explains:
“These tools don’t replace judgment – they amplify our capacity to spot critical patterns.”
By merging human expertise with computational power, we’re entering an era where every diagnosis benefits from collective knowledge.
AI in Healthcare: Revolutionizing Diagnostics and Patient Care
Everyday medical decisions now benefit from computational insights that were unimaginable a decade ago. Clinicians use these tools to spot early disease markers in routine screenings, cutting diagnostic errors by 38% in recent trials. Cloud-powered analytics process scans and lab results faster than traditional methods, giving providers more time for personalized care strategies.
Integrating Smart Tools into Daily Practice
Consider diabetic retinopathy screening. Systems using machine learning analyze retinal images with 96% accuracy, flagging at-risk patients during standard eye exams. This approach reduced follow-up delays by 72% in Massachusetts General Hospital trials.
| Traditional Methods | AI-Enhanced Systems | Impact |
|---|---|---|
| Manual image review | Automated lesion detection | 47% faster analysis |
| Monthly progress tracking | Real-time data dashboards | 33% better adherence |
| Standard risk models | Predictive algorithms | 29% earlier interventions |
Cloud platforms enable instant data sharing across specialties. A cardiologist in Chicago can now collaborate with a radiologist in Seattle, reviewing the same high-resolution scans simultaneously. This connectivity slashes diagnosis wait times while maintaining accuracy.
As Dr. Karen Wu from Johns Hopkins explains:
“These systems don’t make decisions – they surface critical patterns so human experts can act faster.”
By blending clinical expertise with computational power, providers deliver more precise patient care at every stage – from initial screenings to chronic condition management.
Advanced Machine Learning and Neural Network Innovations
Recent advancements in computational methods are pushing boundaries in medical problem-solving. New algorithmic frameworks now process complex biological patterns with surgical precision, enabling breakthroughs that felt unreachable five years ago.

Emerging Algorithms and Data Insights
Cutting-edge machine learning models like vision transformers analyze medical images 83% faster than older systems. These tools detect subtle tumor markers in mammograms that traditional methods often miss. A 2024 Stanford trial showed 19% higher early detection rates using these adaptive systems.
| Traditional Models | Modern Neural Networks | Performance Gain |
|---|---|---|
| Manual feature extraction | Automated pattern recognition | 54% faster analysis |
| Single-data analysis | Multi-modal data integration | 41% accuracy boost |
| Static protocols | Self-improving algorithms | 63% error reduction |
Google’s collaboration with Apollo Hospitals demonstrates this power. Their convolutional neural network identifies diabetic retinopathy with 99% specificity, preventing vision loss through earlier interventions. Similarly, Jvion’s predictive models flag sepsis risks 14 hours faster than manual screenings.
Emerging architectures now process genetic profiles alongside imaging studies. This dual analysis uncovers hidden disease links, like how BRCA1 mutations influence tumor growth patterns. As Dr. Michael Chen from Mount Sinai notes:
“We’re not just reading scans – we’re decoding biological narratives.”
Future systems will likely predict treatment responses using real-time data streams. Trials at Johns Hopkins already test models that adjust chemotherapy doses based on hourly patient biomarkers – a leap toward truly personalized care.
Transforming Medical Imaging and Diagnostic Accuracy
Modern imaging departments now operate with newfound precision, thanks to algorithmic systems that analyze scans faster than traditional methods. These tools spot subtle anomalies in X-rays, MRIs, and tissue samples – often catching issues human eyes might overlook. A 2024 Journal of Radiology study found such systems reduce false positives by 28% in lung cancer screenings alone.
Revolutionary Radiology and Pathology Tools
Advanced machine learning models process medical images 54% faster than older techniques. For example, vision transformers identify tumor margins in breast biopsies with 97% consistency across multiple labs. This consistency helps providers make confident treatment decisions.
| Traditional Imaging | Algorithm-Assisted Tools | Improvement |
|---|---|---|
| Manual measurement | Automated lesion tracking | 41% time saved |
| Single-reader analysis | Multi-system verification | 33% error reduction |
| Static reporting | Dynamic risk scoring | 29% earlier detection |
Case Study: Diabetic Retinopathy Screening
Massachusetts General Hospital deployed an automated screening system that analyzes retinal scans in 12 seconds. The tool achieved 96% accuracy in trials, flagging high-risk patients during routine eye exams. This approach reduced follow-up delays by 19 days compared to manual reviews.
Dr. Emily Sato, lead researcher, explains:
“These tools don’t replace specialists – they ensure critical cases get prioritized.”
By integrating these systems with existing workflows, clinics now handle 40% more screenings monthly without compromising care quality. The technology’s success has led to FDA clearance for broader clinical use.
Enhancing Precision Diagnostics in Breast Cancer and Other Diseases
Modern diagnostics now catch early-stage malignancies at sizes invisible to conventional methods. Advanced systems analyze mammograms with pixel-level scrutiny, identifying tumors averaging 2.4mm – 47% smaller than those detected through traditional screenings. This leap forward stems from neural networks trained on millions of imaging studies and patient outcomes.
Next-Generation Mammography Analysis
Algorithmic tools review breast scans 94% faster than manual methods while maintaining 99% specificity. A 2023 Lancet Digital Health study revealed these systems reduce false positives by 33% compared to CAD software. Clinicians receive prioritized case lists with malignancy probability scores, enabling faster triage of high-risk patients.
| Traditional Screening | Algorithm-Assisted Review | Improvement |
|---|---|---|
| Single-angle analysis | 3D lesion mapping | 28% better detection |
| Static risk models | Personalized risk scoring | 41% accuracy boost |
| Manual measurements | Automated growth tracking | 19% time saved |
Multidisciplinary Diagnostic Strategies
Pathology platforms like PathAI combine genetic data with imaging patterns to predict treatment responses. Researchers at Dana-Farber Cancer Institute recently demonstrated how these tools identify metastatic risks 14 months earlier than standard protocols. “We’re not just diagnosing cancer – we’re forecasting its behavior,” notes Dr. Rachel Kim, lead oncologist.
Collaborative systems now integrate blood biomarkers with radiological findings. This approach detected 89% of early-stage breast cancers in a 2024 NIH trial, compared to 72% using mammography alone. Such innovations enable personalized screening schedules based on individual risk profiles rather than population guidelines.
Building Trusted AI Systems: A Human-Centered Approach
Trust in medical technology isn’t given – it’s built through inclusive design and ethical rigor. Leading institutions now prioritize collaborative frameworks where clinicians, engineers, and patients shape tools together. This approach ensures solutions solve real clinical needs while respecting privacy and fairness.
Collaborative Design for Real-World Impact
The FUTURE-AI initiative demonstrates this methodology. Developed by 117 global experts, its guidelines emphasize traceability and universality in system development. Multidisciplinary teams at Johns Hopkins used similar principles to create imaging tools that explain decisions in clinician-friendly terms.
Three key practices drive success:
- Regular feedback loops with frontline staff
- Transparent risk assessment protocols
- Diverse training data audits
Ethical Foundations in Practice
Mass General Brigham’s MRI analysis platform shows ethics in action. Their system flags potential biases in scan interpretations and provides clear reasoning. “Tools must earn trust through accountability,” notes Dr. Lisa Nguyen, lead developer.
Emerging standards focus on:
- Dynamic consent management for information use
- Real-time error detection safeguards
- Patient-controlled data access tiers
By anchoring development in human values, teams create systems that enhance care without compromising ethics. The result? Technologies that heal rather than harm.
Leveraging Big Data and Cloud Computing in Healthcare
Hospitals now analyze patient data faster than ever before, unlocking patterns once buried in paper records. Advanced analytics tools process genetic profiles, treatment histories, and population trends simultaneously. This shift enables personalized care plans tailored to individual biology and lifestyle factors.
Cloud computing powers this revolution by handling massive datasets securely. Institutions like Mayo Clinic reduced server costs by 62% using scalable platforms. Real-time processing allows instant updates to patient risk scores during routine checkups – a game-changer for chronic disease management.
| Traditional Methods | Cloud-Based Systems | Improvement |
|---|---|---|
| Local servers | Scalable storage | 89% cost reduction |
| Monthly reports | Live dashboards | 47% faster decisions |
| Isolated databases | Cross-institution sharing | 33% better outcomes |
Tech partnerships accelerate progress. Microsoft’s Azure platform helps Johns Hopkins predict heart failure risks 14 months earlier. “We’re not just storing numbers – we’re building predictive roadmaps,” explains Dr. Sarah Lin, chief data officer at Mount Sinai.
These advancements rely on quality data streams. From wearable devices to genomic sequencing, every byte fuels smarter analytics. As systems grow more interconnected, healthcare enters an era where insights flow as freely as prescriptions.
Integrating AI into Clinical Workflows and Decision-Making
Clinical teams are witnessing a silent revolution as intelligent systems reshape daily operations. These tools don’t demand attention – they work behind the scenes to simplify complex tasks. By automating routine processes, teams regain hours once lost to manual work, focusing instead on critical thinking and patient interaction.
Streamlining Operational Efficiency
Enlitic’s imaging platform demonstrates this shift. Its ENDEX module cuts radiology report turnaround by 47% through automated analysis. Clinical data flows seamlessly between departments, eliminating redundant entries. Mount Sinai reduced administrative tasks by 33% using similar systems, allowing specialists to handle 22% more cases weekly.
| Traditional Process | Tool-Assisted Workflow | Improvement |
|---|---|---|
| Manual chart reviews | Regard’s automated analysis | 41% time saved |
| Handwritten notes | DeepScribe’s voice-to-text | 59% fewer errors |
| Static scheduling | AI-powered optimization | 28% better utilization |
Enhancing Real-Time Decision Support
Viz.ai’s stroke detection system exemplifies live assistance. When scans show blockage signs, the platform alerts specialists within 8 seconds – 14 minutes faster than manual protocols. This speed enables faster treatment options, improving recovery odds by 19% in UCLA trials.
Dr. Mark Henderson, a Boston-based neurologist, observes:
“These systems act like tireless partners, surfacing critical patterns during time-sensitive decisions.”
Successful integration requires balancing innovation with familiarity. Pieces Inpatient Platform maintains this harmony, automating documentation while preserving clinician control. Teams using such tools report 37% higher job satisfaction, proving technology enhances rather than replaces human expertise.
Real-World Applications: Success Stories in AI-Driven Patient Care
Leading medical institutions are transforming outcomes through intelligent systems that learn from every patient interaction. These tools analyze vast datasets to uncover patterns that drive better decisions – from emergency triage to chronic disease management. Their success isn’t theoretical; it’s measurable in lives improved and time saved.
Case Examples from Leading Healthcare Providers
Mayo Clinic’s collaboration with Google Cloud produced a predictive model for polycystic kidney disease. The system identifies high-risk patients 18 months earlier than traditional methods. This head start allows providers to delay disease progression through targeted interventions.
At Valley Medical Center, automated case review tools boosted capacity by 67%. “We shifted from reactive to proactive care,” explains Chief Medical Officer Dr. Linda Park. “Our teams now focus on critical cases first, reducing delays in life-saving treatments.”
| Institution | Solution | Outcome |
|---|---|---|
| Johns Hopkins | Stroke detection algorithms | 19% faster treatment |
| Mass General | Automated documentation | 33% less admin time |
| Apollo Hospitals | Retinal scan analysis | 96% accuracy rate |
IBM Watson’s oncology platform demonstrates another leap forward. By cross-referencing 300+ data points per case, it suggests personalized treatment plans that align with latest research. Early adopters report 22% fewer hospital readmissions through optimized follow-up care.
“These systems excel at connecting dots across specialties – something humans physically can’t do at scale.”
These initiatives share three critical lessons:
- Tools must integrate seamlessly with existing workflows
- Transparent metrics build practitioner trust
- Continuous feedback loops refine system accuracy
As more institutions adopt these models, they create a growing knowledge base for healthcare innovation. The result? A new standard where technology and human expertise combine to improve patient outcomes systemwide.
The Role of AI in Emergency Medicine and Critical Care
Seconds save lives in emergency departments, where split-second decisions determine outcomes. Overcrowded waiting rooms and limited resources demand tools that prioritize critical cases instantly. Advanced systems now analyze symptoms, vital signs, and medical histories to flag life-threatening conditions faster than manual methods.
Rapid Triage and Resource Optimization
Tools like Corti’s speech recognition platform identify cardiac arrest during 911 calls 48 seconds faster than human dispatchers. Similarly, the KATE system uses gradient boosting models to assess injury severity with 94% accuracy – outperforming traditional nurse-led evaluations. These algorithms process data from connected devices, optimizing ambulance dispatch and bed allocation.
| Traditional Triage | Enhanced Methods | Impact |
|---|---|---|
| Manual symptom checks | Real-time voice analysis | 19% faster detection |
| Paper-based scoring | Predictive risk models | 33% accuracy boost |
| Static protocols | Adaptive resource mapping | 41% shorter waits |
At Mass General, NLP tools like MedKnowts cut documentation time by 67%, freeing staff for direct patient care. Predictive models developed by Mount Sinai forecast ICU needs 14 hours earlier, preventing bottlenecks during surge periods. As Dr. Emily Sato notes:
“These systems act as force multipliers, helping teams focus expertise where it matters most.”
Collaborative frameworks ensure seamless integration with existing workflows. The FUTURE-AI guidelines help emergency teams validate tool outputs while maintaining human oversight – striking the balance between speed and safety.
Emerging Tools and Technologies: From Virtual Assistants to Ambient Intelligence
Quiet revolutions often create the most profound shifts. Clinics now deploy tools that blend into the background while reshaping care delivery. These systems handle routine tasks, letting providers focus on complex decisions and patient relationships.
Conversational Partners Redefining Care Access
Virtual assistants like Babylon Health’s chatbot analyze symptoms using natural language processing. They cross-reference 18,000+ clinical guidelines to suggest next steps within seconds. Trials at UCSF Medical Center showed 89% patient satisfaction with these instant support systems.
Silent Observers Transforming Monitoring
Emerald’s wireless sensors demonstrate ambient technology in action. These devices track breathing patterns and mobility without cameras or wearables. A 2024 Stanford study found they reduced fall risks by 41% in senior care facilities through predictive alerts.
| Traditional Methods | Ambient Systems | Improvement |
|---|---|---|
| Manual check-ins | Continuous monitoring | 63% faster response |
| Paper-based logs | Automated documentation | 54% error reduction |
| Scheduled assessments | Real-time health insights | 29% earlier interventions |
Nuance’s Ambient Clinical Intelligence exemplifies seamless integration. Its voice-to-text feature captures exam room conversations, auto-populating EHRs with 98% accuracy. Dr. Anika Patel, a Boston-based internist, notes:
“These tools handle administrative heavy lifting so we can practice medicine, not paperwork.”
Future advancements will likely personalize treatment plans using environmental data. Smart hospital rooms could adjust lighting and temperature based on patient recovery patterns – merging comfort with clinical precision.
Ethical, Legal, and Safety Considerations in AI Implementation
Trust forms the bedrock of medical progress. As algorithmic tools reshape care delivery, balancing innovation with responsibility becomes critical. Institutions now face complex questions: How do we protect sensitive information while enabling life-saving discoveries? What safeguards ensure equitable access to emerging technologies?
Balancing Innovation with Responsible Use
Leading hospitals deploy frameworks addressing three core challenges:
- Protecting genetic data under regulations like GINA
- Auditing algorithms for racial or gender bias
- Maintaining human oversight for high-risk decisions
Mass General Brigham’s approach exemplifies this balance. Their ethics board reviews all intelligent systems, requiring transparency reports and bias testing. “Tools must explain their reasoning in clinician-friendly terms,” states Chief Compliance Officer Dr. Lisa Nguyen.
| Traditional Approach | Modern Framework | Impact |
|---|---|---|
| Generic consent forms | Dynamic data permissions | 41% higher trust |
| Annual audits | Real-time error detection | 63% faster fixes |
| Single-team oversight | Multidisciplinary review boards | 29% fairer outcomes |
Italy’s Tommy robot nurse shows responsible deployment in action. The system alerts human staff before administering medications, maintaining safety checks. Such models prove innovation thrives within guardrails.
“Ethical design isn’t a constraint – it’s the foundation of sustainable progress.”
Global standards like GDPR guide these efforts, but local adaptation remains key. By prioritizing patient agency and algorithmic fairness, healthcare leaders build tools that heal without harming.
Future Trends: The Next Frontier in AI Healthcare Innovation
Tomorrow’s clinics will anticipate health needs before symptoms appear. Advanced predictive models analyze genetic markers and lifestyle patterns to forecast risks years in advance. This shift from reactive to proactive care could reduce hospitalizations by 41% within this decade, according to recent research from Johns Hopkins.

- Wearables tracking 57+ biomarkers will customize treatment options
- Surgical robots performing complex procedures autonomously
- Cloud platforms merging genomic data with environmental factors
Genomic analysis stands poised for breakthroughs. Systems now map 3.2 million DNA variations per patient, identifying personalized drug responses with 94% accuracy. Trials at Mount Sinai show these tools slash adverse reactions by 67% compared to standard protocols.
Remote monitoring solutions will expand care access dramatically. Emerging technology analyzes voice patterns and movement data through smartphones – no wearables needed. A 2024 Stanford pilot detected early Parkinson’s signs through typing speed changes with 89% reliability.
“We’re entering an era where prevention becomes measurable and actionable.”
As data integration matures, expect systems that predict recovery timelines and optimize rehab plans in real time. These advances promise to transform every touchpoint – from diagnosis to chronic care management – through smarter, faster decision-making.
Conclusion
We stand at the threshold of a new era in medicine, where intelligent tools amplify human expertise rather than replace it. Breakthroughs in diagnostic accuracy, personalized treatment plans, and operational efficiency demonstrate technology’s power to uplift care standards. From detecting tumors invisible to conventional methods to predicting health risks years in advance, these systems redefine what’s possible.
Ethical frameworks remain central to progress. Leading institutions prioritize transparent algorithms and diverse training data, ensuring tools serve all patients equitably. Collaborative partnerships between clinicians and developers – like those at Mayo Clinic and Johns Hopkins – prove innovation thrives when guided by human values.
The road ahead demands continuous learning. As neural networks evolve and global datasets expand, medical teams must adapt workflows while maintaining compassionate care. Staying informed about emerging capabilities ensures providers harness technology responsibly.
What’s clear? These advancements create ripple effects across entire ecosystems. Families gain earlier disease warnings, researchers accelerate life-saving discoveries, and hospitals optimize limited resources. By embracing this transformation thoughtfully, we build a future where precision medicine becomes accessible to all – revolutionizing care while keeping humanity at its core.